Course
A-Fib and Stroke Risk
Course Highlights
- In this course we will learn about A-Fib and Stroke Risk.
- You’ll also learn about the CHADs Stroke Risk Scoring System.
- You’ll leave this course with a broader understanding of how oral anticoagulants are used to reduce stroke risk in patients with A-FIb.
About
Contact Hours Awarded: 1.5
Course By:
Marybeth A. Keppler
RN, BSN, OCN, M.Ed
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
In 2023, stroke was the third leading cause of death in the United States after heart disease and cancer (1). As the life expectancy of the average American is approximately 76 years (2), an increasing number of people will live with comorbid health conditions compared with prior generations. One risk factor for stroke, apart from high blood pressure, is atrial fibrillation (also known as AFib or AF), which causes approximately 15% of strokes (3). Furthermore, people living with AFib are up to five times more likely to have a stroke than those without this condition (4). Nurses are critical providers of education and information to patients about their risk of AFib and stroke. They can elucidate a deadly subject to help patients reduce their risk of morbidity and mortality.
Pathophysiology of A-Fib and Stroke
Atrial fibrillation, the most common arrhythmia, is due to rapid or disordered electrical signals in the heart's upper chambers (the atria). These impaired signals cause the atria to contract too chaotically and quickly, termed fibrillation. AFib causes blood to pool in the atria and increases the risk of blood clots, stroke, and heart disease (15).
Since AFib can exist in asymptomatic patients, estimates of its prevalence vary between 3 to 6 million Americans, with 12 million patients affected by the year 2030 (15). Worldwide, that number is estimated at over 33 million, or approximately 0.5% of the planet’s population, though numbers are likely far higher due to the underdiagnosing of the condition (15). Within the United States, AFib is directly linked to nearly 160,000 deaths per year (15, 16). Part of the reason AFib is so deadly is that 1 in 7 strokes are caused by this condition (16).
Strokes occur when blood vessels in the brain rupture (hemorrhagic) or are blocked by a clot (ischemic). These incidents reduce blood flow to the brain, affecting the transport of essential elements like oxygen and nutrients for cell survival. Ischemic strokes occur in approximately 87% of cases (5).
Strokes originating from cardiac factors like AFib are known as cardioembolic; AFib is one of the major causes of cardioembolic strokes (6). Approximately 20-25% of ischemic strokes are cardioembolic in nature, their incidence increasing with age (6,8). A cardioembolic stroke occurs when blood clots or emboli travel from the heart or aorta and lodge in the cerebral circulation, causing ischemia. The risks of both AFib and stroke grow with age, and when the two conditions occur together, the results of the stroke are usually more severe and deadly (7, 8, 15).
While AFib is the highest contributor to cardioembolic stroke, other causes include sick sinus syndrome, structural diseases (like patent foramen ovale), valvular heart disease (such as infective endocarditis and valvular calcifications), septal or ventricular aneurysms, heart failure with reduced ejection fraction (HFREF), and myocardial infarction (MI) (6).
The course of illness depends on the severity of the stroke, pre-existing conditions, age, and any other complications present. Stroke generally presents rapidly and is a medical emergency. Most hospitals require patient education regarding stroke signs, symptoms, and management, such as when to call for EMS promptly.

Self Quiz
Ask yourself...
- Have you ever had a patient/client who had difficulties maintaining anticoagulation regimens and lab follow-up? Did they ever present with clotting disorders such as DVT, PE, or Stroke?
- TEE and/or Echocardiogram exams are often ordered by practitioners for patients in A-Fib. If a thrombus was found within the heart's upper chambers, would this be a critical result to be reported immediately? What treatment can you anticipate?
Risk Factors for A-Fib and Stroke
In general, the risk factors of cardioembolic stroke overlap with the general risk factors for stroke and include hypertension, diabetes mellitus, hyperlipidemia, cardiac diseases, and lifestyle factors. When educating patients with AFib about their risk of developing a stroke, numerous risk factors may be considered for teaching opportunities.
The following chart shows modifiable versus non-modifiable risk factors for AFib that lead to stroke (9,10,11,15):
| Modifiable | Non-Modifiable |
| Hypertension | Age (older than 65 years) |
| Hypercholesterolemia | Race (higher risk of AFib for those of European descent; higher risk of stroke fr African Americans) |
| Rheumatic heart disease or pericarditis |
Sickle Cell Anemia |
| Metabolism Syndrome, Diabetes Mellitus, Hyperthyroidism | Prior stroke, TIA, or MI |
| Poor diet |
History of migraine headaches |
| Heart Disease (A-fib, valve disease, prosthetic valve, mitral stenosis) | Sex (men have a higher risk of AFib; women for stroke) |
| Excessive alcohol or caffeine consumption alcohol | Family History |
| Smoking or other tobacco use |
|
| Sleep apnea |
|
| Obesity | |
| Physical inactivity | |
| Carotid or peripheral artery disease |
|
| Athleticism (higher incidence of SVT, which can lead to AFib) | |
| Lung or Kidney Disease | |
| High-stress levels or mental health conditions |
The clinical team must work with the patients and families to identify the specific risk factors for each patient to reduce the risk of stroke.

Self Quiz
Ask yourself...
- Do any of these risk factors surprise you?
- Are patients always aware or forthright regarding their risk factors?
CHADs and Stroke Risk Scoring in A-Fib
Cardiologists and other clinicians use a scoring system to evaluate the stroke risk for those with atrial fibrillation. The CHADS2 score was first published in 2001 and stands for Congestive heart failure, Hypertension, Age ≥75 years, and Stroke [Double weight] (12). Its goal is to predict the risk of stroke in patients with nonrheumatic AFib, and the score assists practitioners in making anticoagulation decisions (12).
Patients with high scores (>2) are at significant risk for stroke: They have a 5.9% annual risk with a score of 3 and as high as an 18.2% yearly risk for those with a score of 6 (12). The CHADS2 did not include some additional risk factors for stroke. It was revised to the CHA2DS2-VASc, which contains three more risk factors: vascular diseases (e.g., coronary artery disease and aortic atherosclerosis), age (65-74 years old), and female sex (12). See tables below (12).
CHADS2 Score: Stroke Risk Assessment in Atrial Fibrillation: (4)
| Score | CHADS2 Risk Criteria |
| 1 point | Congestive heart failure |
| 1 point | Hypertension |
| 1 point | Age ≥ 75 years |
| 1 point | Diabetes mellitus |
| 2 points | Stroke/transient ischemic attack |
CHADS2 Score and Corresponding Annual Stroke Risk: (4)
| CHADS2 Score | Adjusted Stroke Risk (%) |
| 0 | 1.9 |
| 1 | 2.8 |
| 2 | 4 |
| 3 | 5.9 |
| 4 | 8.5 |
| 5 | 12.5 |
| 6 | 18.2 |
CHA2DS2-VASc Score and Risk Criteria: (4)
| Score | CHA2DS2-VASc Risk Criteria |
| 1 point | Congestive heart failure |
| 1 point | Hypertension |
| 2 points | Age ≥75 years |
| 1 point | Diabetes mellitus |
| 2 points | Stroke/Transient Ischemic Attack/Thromboembolic event |
| 1 point | Vascular disease (prior MI, PAD, or aortic plaque) |
| 1 point | Age 65 to 74 years |
| 1 point | Sex category (i.e., female sex) |
The American Heart Association/ American College of Cardiology/ Heart Rhythm Society (AHA/ACC/HRS) considers recommending oral anticoagulants to patients who have a CHA2DS2-VASc score of 1; at a score of 2 or higher; the recommendation is certain (14).

Self Quiz
Ask yourself...
- Would explaining the risk for stroke CHADS2 scoring system to patients and families assist them in making decisions about anticoagulants?
- What are the common concerns that patients and families have regarding taking "blood thinners"?
Case Study
John, a 76-year-old Caucasian male patient, presents to the ED with cellulitis, intermittent heart palpitations, and shortness of breath. He has a history of diabetes mellitus and peripheral arterial disease with right-toe amputation. John quit smoking two years ago after a 60-pack-year history. His vital signs upon presentation are Temp: 38.1°C, HR 130, BP 150/88, RR 16, SpO2 94% on room air. His ECG rhythm reads atrial fibrillation, and he states he had never been told he had this condition before.
He did not want to come to the hospital, but his wife Sally insisted since his cellulitis wounds started spreading and weeping. Sally states that John has seemed tired and irritable lately and has endorsed some new-onset lightheadedness and shortness of breath at rest. He is treated with broad-spectrum IV antibiotics and moderate-rate fluid replacement. Cardiology was called to evaluate the AFib.

Self Quiz
Ask yourself...
- Using the CHA2DS2-VASc risk scoring system what would his score be?
- Would he qualify for oral anticoagulants?
- Would IV heparin infusion be considered in his case?
Oral Anticoagulants in A-Fib and Stroke Reduction
Patients with AFib-induced stroke will have an anticoagulation regimen prescribed, likely along with other treatments, whether newer or traditional; anticoagulants on the market can be confusing and difficult for patients to differentiate when evaluating risks and benefits.
There are many oral anticoagulants available now, each with its unique properties. If warfarin (Coumadin) is used, the INR goal is generally around 2.5. However, there are situations, especially in the over-75 age group, where a lower INR goal of 2.0 is acceptable (13). Warfarin has an onset of 36-48 hours and can last in the system for 2-5 days, delaying any surgical procedures. Other oral anticoagulants for atrial fibrillation include apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), and rivaroxaban (Xarelto). Each has a unique drug profile, half-life, and reversal agent.
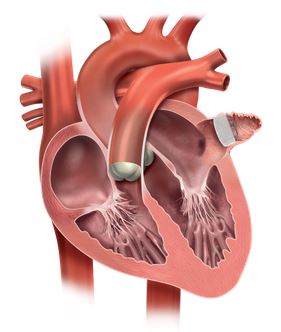
For those unable to take anticoagulants and at risk for atrial thrombus (which can form in the left atrial appendage due to reduced contractility during AFib), a device called the Watchman has been created. It is a tent-like device surgically placed in the left atrial appendage to seal it off. Since more than 90% of stroke-causing clots come from the left atrial appendage in nonvalvular AFib, the Watchman aims to significantly reduce the risk of clots at that site (13). The outpouching of the sac is seen protruding from the left atrium in the diagram below (13).
Other treatments for AFib include lifestyle changes, medicines, surgery, and other procedures that aim to slow and restore the heart's regular rhythm and help prevent blood clots (15). In addition to the oral anticoagulants listed above, other medications may include beta-blockers (e.g., atenolol and metoprolol), calcium channel blockers (e.g., diltiazem and verapamil), and digoxin (15). If those treatments fail to treat the AFib effectively, other medications like amiodarone, dofetilide (Tikosyn), flecainide, procainamide, and others may be given, but they all require careful monitoring and dosing (15). Surgical and procedural treatments generally include electrical cardioversion, AV node ablation, and implanted pacemakers (15).
Ways to prevent the risk of stroke in people with AFib include, but are not limited to (15):
- Controlling blood pressure, cholesterol and triglyceride levels, and weight
- Taking all medications as prescribed and informing the primary care provider of any other drugs or herbal supplements used
- Eating a diet low in saturated and trans fats and high in fruits, vegetables, and whole grains
- Getting daily exercise of at least 30 minutes
- Quitting smoking and reducing alcohol and caffeine consumption
- Maintaining overall health by scheduling regular physical examinations
- Monitoring and treating other comorbidities
- Reporting all instances of dyspnea or angina immediately to a physician
Conclusion
By the nature of atrial fibrillation, all patients with this condition have risk factors for stroke. The clinical team's responsibility is to assess each patient’s unique risk and then educate them in making decisions regarding stroke prevention. The risk of stroke from atrial fibrillation is a genuine concern as the population ages, and the number of patients diagnosed with these comorbid conditions is on the rise.
For patients presenting with ischemic stroke, the causal factors must be investigated to prevent stroke reoccurrence, which will likely include proper management of anticoagulants for atrial fibrillation. The nurse is responsible for providing information and resources for the patient to manage these conditions. As part of ongoing care, the nurse can also help reduce morbidity and mortality in patients who might otherwise succumb to AFib and stroke.
References + Disclaimer
- Centers for Disease Control and Prevention, National Center for Health Statistics (2024). National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. http://wonder.cdc.gov/mcd-icd10-provisional.html
- Centers for Disease Control and Prevention. (2023). Deaths and Mortality. https://www.cdc.gov/nchs/fastats/deaths.htm
- The American Heart Association (2023). High Blood Pressure, Atrial Fibrillation and Your Risk of Stroke. https://www.heart.org/en/health-topics/atrial-fibrillation/why-atrial-fibrillation-af-or-afib-matters/high-blood-pressure-afib-and-your-risk-of-stroke
- Shah, A. (2023). What you may need to learn about AFib and stroke. https://www.uchicagomedicine.org/forefront/heart-and-vascular-articles/what-you-may-not-know-about-afib-and-stroke
- Johns Hopkins Medicine (2024). Types of Stroke. https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/types-of-stroke
- Pillai, A. A., Tadi, P., & Kanmanthareddy, A. (2024). Cardioembolic Stroke. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK536990/
- Vinding, N. E., Kristensen, S. L., Rørth, R., Butt, J. H., Østergaard, L., Olesen, J. B., Torp‐Pedersen, C., Gislason, G. H., Køber, L., Kruuse, C., Johnsen, S. P., & Fosbøl, E. L. (2022). Ischemic Stroke Severity and Mortality in Patients with and Without Atrial Fibrillation. Journal of the American Heart Association, 11(4), e022638. https://doi.org/10.1161/JAHA.121.022638
- Elsheikh, S., Hill, A., Irving, G., Lip, G. Y. H., & Abdul-Rahim, A. H. (2024). Atrial fibrillation and stroke: State-of-the-art and future directions. Current Problems in Cardiology, 49(1, Part C), 102181. https://doi.org/10.1016/j.cpcardiol.2023.102181
- American Stroke Association. (2023). Risk Factors Under Your Control. https://www.stroke.org/en/about-stroke/stroke-risk-factors/risk-factors-under-your-control
- American Stroke Association. (2023). Stroke Risk Factors Not Within Your Control. https://www.stroke.org/en/about-stroke/stroke-risk-factors/stroke-risk-factors-not-within-your-control
- American Stroke Association. (2023). Who is at Risk for Atrial Fibrillation? https://www.stroke.org/en/health-topics/atrial-fibrillation/who-is-at-risk-for-atrial-fibrillation-af-or-afib
- Tarek, A., & Mehdirad, A. A. (2022). CHADS2 Score for Stroke Risk Assessment in Atrial Fibrillation: CHADS2 and CHA2DS2-VASc Score for Stroke Risk Assessment in Atrial Fibrillation. https://emedicine.medscape.com/article/2172597-overview
- Hull, R. D., & Garcia, D. A. (2023). Management of warfarin-associated bleeding or supratherapeutic INR – UpToDate. https://www.uptodate.com/contents/management-of-warfarin-associated-bleeding-or-supratherapeutic-inr
- com (2024). Afib Stroke Risk and Prevention—Reduce Stroke Risk with WATCHMAN. https://www.watchman.com/en-us/atrial-fibrillation-stroke.html
- Thomas, J. (2023). Facts and Statistics About Atrial Fibrillation. https://www.healthline.com/health/living-with-atrial-fibrillation/facts-statistics-infographic
- Centers for Disease Control and Prevention (2022). Atrial Fibrillation. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

